6 Crucial Tips for Successful Bed Sore Treatment
This article first appeared on Vive health’s blog.
Bed sores are, unfortunately, one of the most common ailments resulting from mobility issues. It’s important to begin bed sore treatment at the first sign of any symptoms. Pressure ulcers are much easier to deal with when they’re caught early. Even better, if you understand a risk is present, you can take precautions to reduce the likelihood of occurrence.
Your healthcare provider will want to examine the affected area or areas when diagnosing suspected bed sores. Surgery is usually not recommended as long as you have not progressed into later bed sore stages.
Here are simple tips to try that you can discuss with your healthcare provider:
1. Frequent Repositioning
If you are in a chair, wheelchair or bed for a long period of time, you need to vary your position – This will help to facilitate blood flow and reduce pressure on your boney areas so you are less likely to get a bed sore. It is important to be regularly repositioned so the pressure is dispersed throughout the body.
Wheelchair Repositioning
- Try shifting your weight by yourself every 15 minutes or so. Go from left to right side of your buttock as well as shifting your position further forward or backward in your chair.
- Consider a wheelchair or seat cushion to help re-distribute pressure across your bottom (high-risk area). Avoid donut shaped cushions as they reduce blood flow to bottom increasing risk.
- Consider a tilting, specialty wheelchair. These are expensive, but depending on your budget and access to a caregiver, they can be worth it.
Bed Repositioning
- Adjust position frequently. Adjust between your left side, right side and back, ideally switching positions every 1-2 hours.
- Consider a bed side rail to assist you with repositioning if you are unable to change positions without assistance.
- If possible, adjust the elevation of your bed. Do not raise it to more than 45 degrees to avoid too much pressure on the tailbone or possibility of shearing.
- Alternating pressure mattresses provide automation to constant repositioning. Air compartments inflate or deflate (usually in 6-minute intervals) to reposition pressure areas across the body. Alternating pressure mattresses come in 2 categories you can look into. Alternating pressure mattress overlay – pressure mattress gets placed on top of your regular or medical mattress. The overlay pad accommodates any sized mattress and can be secured underneath fitted sheets. An Alternating pressure mattress replacement – is a complete mattress replacement that goes on top of a medical bed frame. More robust system with low air loss.
2. Proper Dressings and Wound Care
Proper dressing and cleaning of the pressure ulcer is essential. Open wounds are particularly prone to infection. Appropriate care and use of dressings will promote healing and shield bacteria.
(Always avoid using hydrogen peroxide as it can further damage the skin.)
Proper care for bed sores is determined by the stage of the pressure sore:
**Special treatment gels, foams, and dressings are available but discuss with your doctor which would be best for the condition of your bed sore.
3. Proper Nutrition
Making good food choices will help facilitate healing and help prevent future bed sores. Foods rich in vitamins A, C and E are ideal. Consider oranges, strawberries, tomatoes, broccoli, cauliflower, nuts, olives (and olive oil for cooking) as a good starting point.
Nutritional drinks, such as Juven, support wound healing and can be incorporated into your bed sore treatment. Vitamin C, Zinc, and Omega-3s are also great supplements to include in your diet for tissue repair. (These supplements are available OTC, but remember to discuss with your doctor before starting your own regimen.)
Maintaining a healthy weight is is frequently overlooked. In many cases, bedridden patients lose bodyweight. This means less protection between skin and bone. Conversely, with excess weight there will be more pressure on the body creating a higher risk. Do your best to monitor your weight and make sure you are maintaining a healthy balance.
Advanced pressure ulcers can possibly be treated directly or orally with antibiotics – this would be something that your healthcare provider would discuss with you if he or she feels it’s necessary.
4. Prevent Further Injury or Shearing
Pressure ulcers and sensitive skin are susceptible to further injury with very minor force. You are at increased risk of damage from friction during repositioning or other basic movements.
Make sure to apply powder to your sheets to reduce friction. Do not engage in unnecessary exposure to pressure in sore areas. Keep your skin as moisturized as possible by staying hydrated and get the ok from your doctor to utilize barrier cream.
5. Incontinence Management
Limited mobility combined with incontinence makes for a heightened risk of infection, particularly with open wounds. Diapers and bed incontinence pads need to be used to reduce bacteria exposure to skin. Protective lotions can also be used to shield the skin. In severe cases, catheters or rectal tubes may be necessary, please consult with your healthcare provider for details.
6. Change Bedding and Clothing Frequently
A fresh set of clothes and sheets makes everyone feel better. A clean environment is especially important when bed sores or a risk of bed sores are present. During daily checks of the skin, make sure to change clothes and sheets to limit the ability for bacteria to spread. Try to time body inspection with clothing and sheet changes to avoid exposure to additional shearing or friction.
**Sheets and clothes should be made of cotton or breathable fabric. Some flannel or jersey materials are too dense, restricting airflow, and in turn, inhibit healing.
Avoiding Pressure Ulcers in Wheelchair
Dealing with the risk of pressure ulcers for wheelchair bound patients requires a slight variation in care and there are a few specifics you NEED to know.
1. Is your wheelchair the proper size and fit?
Factors to consider:
- Amount of mobility
- posture
- discomfort level
- inhibiting conditions
(please consult with your primary care physician before making your final selection)
Weight Restrictions:
Measure weight to ensure that desired wheelchair can properly support patient. Also keep in mind the weight of the chair. If you need a chair that can be easily transported, a lightweight design may be more appropriate.
The Seat:
Determine the necessary seat width you will need.
It’s recommended that you measure width of patients hips and then add 2 inches.
Next, you need to find the appropriate depth, measure from the back of the hip to the back of the knees and subtract 1 inch.
The Backrest:
Additional back support can be provided by certain wheelchair designs. Again, assess the intended patient’s condition and necessities to determine most comfortable fit.
**With person seated in wheelchair, measure from collarbone to seat.
The Footrest:
Determine what special features may be needed. Some patients require their legs to be lifted, and there are different size variations based on user’s height.
**Measure from the back of the knee to heel of the foot
The Armrests:
You may not have realized that wheelchairs are available with different armrest and height variations.
**The height of your armrests should be determined by measuring from the elbow to seat of chair with arms up and bent at 90-degree angle
Full-Length -> ideal for having to perform standing or pivoting transfers and provides surface that allows to additional push and support.
Desk-Length -> designed for patients who spend time sitting at a surface or desk, and allow for you to comfortably get closer.
2. Check for proper fit at least twice a year
The patient may gain or lose weight over the course of time which can compromise the proper fit.
Take note of any painful areas, and let your doctor know immediately!
3. Repositioning
Shift weight to take pressure off of certain areas and promote blood flow. Leaning forward and side to side are the easiest movements
Caregivers must assist with shift weight every 15-20 mins. We realize that this can be very overwhelming to manage and almost unrealistic
So consider the use of medical aids. Just like bed sores, treatment for pressure ulcers from a wheelchair can be enhanced with the use of alternating pressure pads or cushions.
WARNING: Do not utilize “donut” hemorrhoid cushions
(these are not designed to reduce pressure points and can worsen your condition)
What are Bed Sores?
A bed sore is an area on your skin that is irritated and painful due to prolonged pressure.
One of the very beginning signs of a developing bed sore is sore skin. Light skin tones will show that area is red, discolored, or darkening; while darker skin tones present purple, blueish, or shiny areas. If untreated, these spots generally turn hard and warm to touch as they progress into stage 2 ulcers. Pressure ulcers are categorized in stages from 1 to 4, stage 1 being least severe and stage 4 being most severe.
Stages of Pressure Ulcers
Pressure sores are categorized in one of four ways:
Stage One
Your skin is discolored, but not broken. If you have a light complexion, the pressure ulcer may appear red or could look blue or purple. If you have a dark complexion, it may look white.

Stage Two
Your skin has a break in it and there may be some dead skin around the wound. You may also notice a reddish-pink area in the center, which could also involve a blistered area.

Stage Three
The pressure ulcer takes on the appearance of a crater and may go into your fat layer. The pressure sore may also have some pus or drainage.

Stage Four
A bed sore that is this deep involves your muscle, bone and possibly tendons and joints. Your healthcare provider may also notice a substance referred to as eschar.

In extreme cases, a bed sore may actually be unstageable , but this is rare if you’re seeking treatment. In this particular case, the tissue layers involved would need to be surgically removed.
Risk Factors
People who have the highest risk for bed sores are typically:
- Bedridden
- Spend most of their day in a wheelchair
- Incontinent
- The elderly (due to decrease skin elasticity)
- Diabetic
- Have fragile skin
If you are at risk for bed sores it is important you implement a prevention plan. Movement is the best way to avoid bed sores. Make sure you stay as active as possible, try to schedule fixed times for position changes and exercise into your daily routine.
It’s also important to make sure that you eat properly and drink plenty of water. Poor nutrition can increase your chances of getting pressure sores, especially if you aren’t getting enough vitamin C, protein and zinc.
Those who smoke are also at a higher risk for bed sores. Nicotine will hinder your circulation and slow your healing process.
Bed Sore Causes
When there is too much pressure on your skin for an extended period of time, it diminishes the blood flow to that area. This increases your chances of developing a pressure ulcer. A couple of other causes are:
If you have frail, thin skin, a bruise or a scrape can lead to a pressure sore.
The friction to your skin that can come from a wheelchair that is an improper fit, or the head of your bed raised too high.
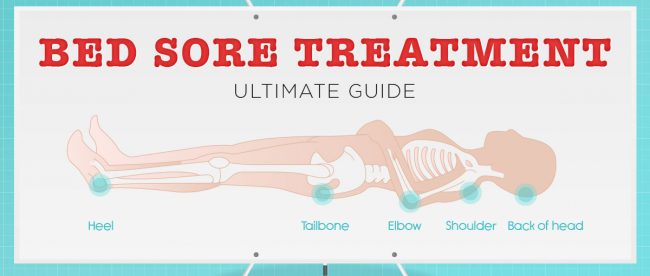
Bed – Most vulnerable parts of body for pressure ulcers
- Tailbone
- Back of Head
- Buttocks
- Shoulders
- Heels
- Backs of arms or legs
- Spine
- Ankle
- Knee

Wheelchair – Most vulnerable parts of body for pressure ulcers
- Shoulder Blade
- Buttocks
- Heel
- Ball of Foot

Complications:
Ignored or improperly treated bed sores can lead to some very scary complications.
-Pressure ulcers that advance to stage 3 & 4 can become life threatening and require attention immediately.
-Lack of treatment may lead to amputations of affected areas
-Infections can spread to other areas of the body such as your blood, heart, and bones
What’s next?
STICK TO THE PLAN!
It’s important to follow a routine bed sore treatment plan.Take the time to consistently apply the regimen you and your healthcare provider have put together using our treatment tips and recommended products. Remember, knowing how to treat bed sores will help to prevent future ones. This will be your best line of defense for bringing about the quickest recovery and return to your best quality of life.
Source: Vive health

Leave a comment